What is Acute Myeloid Leukemia (AML)?

Rally Kid Maylee fought AML twice by age seven. Though she was diagnosed with Graft Versus Host Disease (GVHD), she is beating cancer.
Acute myeloid leukemia (AML) is a blood cancer of the myeloid cells that normally form white blood cells, red blood cells or platelets. AML originates in the bone marrow, where the leukemia cells build up and overcrowd normal cells. The leukemia cells often move into the bloodstream fairly quickly.
AML is the second most common form of childhood leukemia, after acute lymphoblastic leukemia (ALL). AML is much more common in adults versus children; the average age of diagnosis is 68. There are only about 500 childhood AML cases in the U.S. each year, compared to more than 19,000 in adults. Alternatively, far more children are diagnosed with ALL compared to adults.
Down syndrome is associated with a higher risk of both ALL and AML in children. AML is more sensitive to chemotherapy in children with Down syndrome compared to those without, which leads to a better prognosis—especially if the child is diagnosed prior to the age of four.
ACUTE MYELOID LEUKEMIA SIGNS AND SYMPTOMS
“Children diagnosed with AML often have multiple symptoms that are severe, not explained by other causes, and persist for weeks,” said Rally-funded researcher and Career Development Award Winner, Benjamin Huang, MD, Assistant Professor of Pediatrics and Attending Pediatric Hematologist/Oncologist at University of California San Francisco. “A few of these symptoms include fatigue or pallor, extensive or large bruising, and unexplained and persistent fevers.”
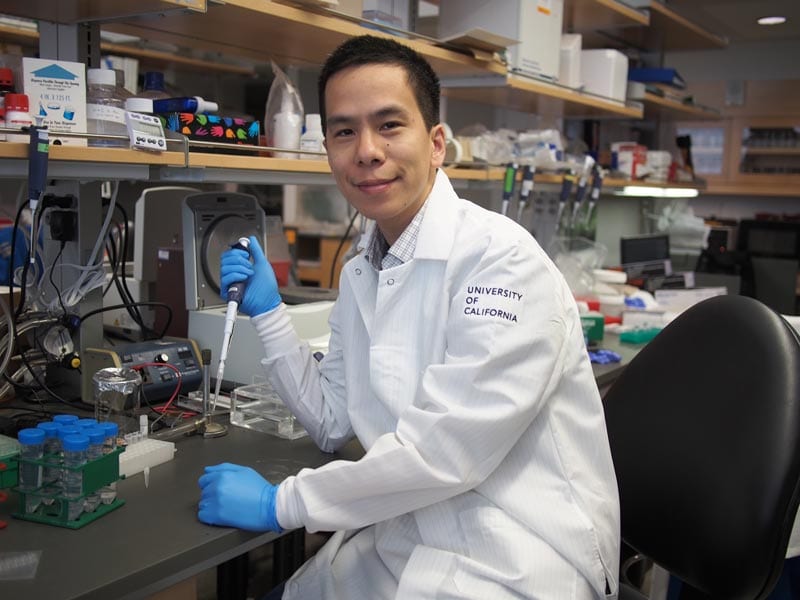
Dr. Huang hopes to develop a novel test that harnesses “best in class” technologies to enable detection of one leukemia cell for every one million normal cells—a sensitivity that eclipses the current standard of care by more than one hundred-fold.
Additional symptoms of AML may include:
- Pain in the back, legs or joints
- Trouble standing or walking
- Persistent headaches
- Ongoing infections
- Frequent or severe nose bleeds, bleeding gums, unexplained rash
- Loss of appetite with or without weight loss
- Swollen lymph nodes
- Swollen or tender stomach, liver or spleen
- Trouble breathing
It’s important to remember that other conditions can cause similar symptoms, so having any one of these does not mean that a child has blood cancer or AML.
ACUTE MYELOID LEUKEMIA DIAGNOSIS, TREATMENT AND PROGNOSIS
AML is diagnosed via a blood test as well as a bone marrow aspiration and biopsy. During this procedure, a needle is inserted into a large bone—usually the hip or pelvis—to remove a small amount of liquid bone marrow and a piece of the spongy tissue inside the bone. AML is diagnosed when the bone marrow contains 20% or more immature myeloid cells, called myeloblasts or myeloid blasts.
Additional chromosomal tests are performed to reveal the exact AML subtype. AML has many subtypes, based on the type of bone marrow the cells come from, how mature the cells are and if the cells have specific genetic markers or chromosomal abnormalities.

Rally Kid Mikey was diagnosed with AML at age seven. He relapsed the following year and is still dealing with side effects from his bone marrow transplant and GVHD.
Generally, treatment for AML uses higher dosages of chemotherapy (chemo) for less than a year. Chemo is given intravenously, into muscle, in the cerebrospinal fluid (CSF) and/or orally. AML is treated with a combination of several chemo drugs such as vincristine, L-asparginase, daunorubicin, methotrexate, Idarubicin, 6-mercaptopurine, doxorubicin, cytarabine and/or cyclophosphamide. Steroids like prednisone, prednisolone, dexamethasone and hydrocortisone are also often used as well.
“The chemo that is used is really intense and can have significant side effects—high risk for infection, mouth sores, fevers, skin rashes, damage to the heart and liver. It would be great to be able to develop new treatments that are more specific to AML cells and that spare normal cells in the body,” said Rally Medical Advisory Board Member, Daniel Wechsler, MD, PhD, Director of Pediatric Oncology at Children’s Healthcare of Atlanta and Professor, Department of Pediatrics at Emory University.

Rally Kid Anna Charles, aka AC, was diagnosed with AML at age six. She fought bravely for five months, becoming paralyzed from the waist down as a result of surgery, before she sadly passed away.
Treatment of AML is divided into two phases: induction and consolidation.
The induction phase is usually two or three cycles of chemotherapy over the course of five to seven days each. Approximately 85% to 90% of children with AML achieve remission after this phase.
The consolidation phase uses more intensive treatment to kill any remaining leukemia cells. For those children who do not reach remission through chemotherapy, a stem cell/bone marrow transplant may be recommended.
“Over the past 25+ years, I have taken care of many AML patients,” said Dr. Wechsler. “Unfortunately, the cure rates for AML have not really improved much—patients with AML have a 50-60% chance of being cured, similar to cure rates in the 1990’s.”
ACUTE MYELOID LEUKEMIA RESEARCH
Thankfully, progress is being made to improve the outcome for children diagnosed with AML. However, there is much work left to be done.
“The more we learn about AML, the more we are finding that not all AML’s are the same, and that in fact each AML contains its own unique genetic signature. As the next generation of therapeutic strategies are being developed, accounting for these genetic differences and predicting how a patient’s AML will respond to these new therapies is paramount to improving cure rates,” said Dr. Huang.
Rally Kid Jordan was first diagnosed with AML in middle school then relapsed in college. He is now a cancer-free young adult!
“I cannot emphasize enough the importance of research funding and participation, as past and current advances are only possible through rigorous scientific testing and clinical trial research,” said Dr. Wechsler. “There are new drugs that specifically attack AML cells that are being tested, and Precision Medicine—using DNA sequencing to identify specific changes in an individual patient’s AML leukemia cells and then choosing drugs that will work specifically against that patient’s leukemia—is becoming more widely available.”
JOIN THE FIGHT AGAINST ACUTE MYELOID LEUKEMIA
Children with acute myeloid leukemia need continued research for better treatments. Rally Foundation is funding some of the most innovative and cutting-edge blood cancer research.
“I envision a direct path from the research supported by the Rally Foundation to more effective therapeutic approaches for pediatric patients with AML.” – Dr. Huang
Give in honor of kids like Maylee, Mikey, AC and Jordan and make a donation to AML research today.

0 Comments
Trackbacks/Pingbacks